In 2009 a novel influenza strain, A H1N1 California 7/09 (pH1N1), “swine flu”, emerged in Mexico and rapidly spread worldwide. Although generally causing mild disease, pH1N1 resulted in severe illness in some individuals. On 11 June 2009 the WHO officially declared an influenza pandemic in recognition of the global impact of the novel strain. (World Health Organization, 2005; Bishop, J., 2009)
The Australian public health response to pH1N1 was aimed at protecting individuals and mitigating the impact on social function and the economy. (Australia Government Department of Health and Ageing, 2009) Initially, containment phase plans in Australia were focussed on limiting transmission through social distancing measures and the widespread use of antiviral drugs for both prophylaxis and treatment. However, with the escalation of local transmission and evidence suggesting that disease was not as serious as initially believed, the containment measures were relaxed while awaiting the development of a tailored vaccine, focussing on early treatment of individuals with underlying high-risk conditions. (Eastwood, K., et al, 2009)
In Australia, following safety and efficacy trials, a pH1N1-specific vaccine was registered by the Therapeutic Goods Administration in September 2009. Health authorities agreed that given the decrease in pH1N1 disease activity the use of mass clinics was not immediately necessary and that the rollout could be achieved principally through general practices and existing public health services. Whilst stated willingness to accept the vaccine is reportedly high the actual uptake thus far is unlikely to achieve adequate ‘herd immunity’. (Eastwood, K., et al, 2009) Should a second pandemic wave occur or mutation resulting in a strain with more serious health consequences, then mass vaccination delivery through community clinics will need to be considered.
Although real-time field exercises are considered the gold standard for evaluating disaster response capabilities, until now, no Australian State or Territory had tested the effectiveness of their mass vaccination plans by field exercise. (Aaby, K., et al, 2008) In this report we describe our experiences in conducting a large field exercise in March 2008 in which we provided seasonal influenza vaccine to a circumscribed rural community of 1800 people in the Hunter Valley, NSW, which included the town of Aberdeen. Our aim was to provide the current seasonal influenza vaccine rapidly and safely. Two key summary measures of mass clinic effectiveness are clinic capacity (the number of patients successfully vaccinated per hour) and throughput time (time spent by a patient in the clinic). (World Health Organization, 2008) The exercise tested the NSW pandemic influenza mass vaccination clinic response protocols. (New South Wales Health, 2005)
The aim of this exercise was to evaluate and refine mass vaccination clinic plans under the NSW Health Interim Influenza Pandemic Action Plan. The exercise assessed the capacity of the existing Plan to efficiently and safely implement a local mass vaccination clinic operational plan and evaluate the capacity to deliver adequate and timely treatment of mass presentations. The Hunter New England Human Research Ethics Committee considered the exercise a quality assurance exercise and formal ethics approval was not required.
The coordinating group consulted extensively with Local Emergency Management Committee (LEMC) representatives, the Upper Hunter Shire Council, the local Division of General Practice, the town’s general practitioner, the local school which provided the venue, security contractors and local volunteer organisations. Additionally, local hospital staff and community nurses participated in the exercise.
The Philadelphia Health Department, USA, provided valuable advice from their previous experiences of mass drug distribution. (Philadelphia Department of Public Health Division of Disease Control, Bio-terrorism and Public Health Emergency Preparedness Consultants, 2005) For staff participating in the clinic, multi-agency training and briefings were conducted in the weeks prior to the exercise. The Chief Umpire was the Local Emergency Operations Controller (LEOCON), a senior officer from the local Police Command, who was supported by seven umpires/evaluators from NSW Health and three NSW Area Health Services.
The target population was approximately 1800 individuals representing the entire postal code cohort of individuals aged greater than 6 months. Children aged 6 months to 9 years who had not received an influenza vaccine in previous years were offered a second influenza dose six weeks after the exercise.
After Action Reviews (AARs) were convened immediately following the exercise to solicit key points of impact in the running of the exercise. A strategic consultative meeting with NSW Health’s Biopreparedness and Immunisation Units was convened two months following the exercise to agree on protocol changes identified by exercise findings.
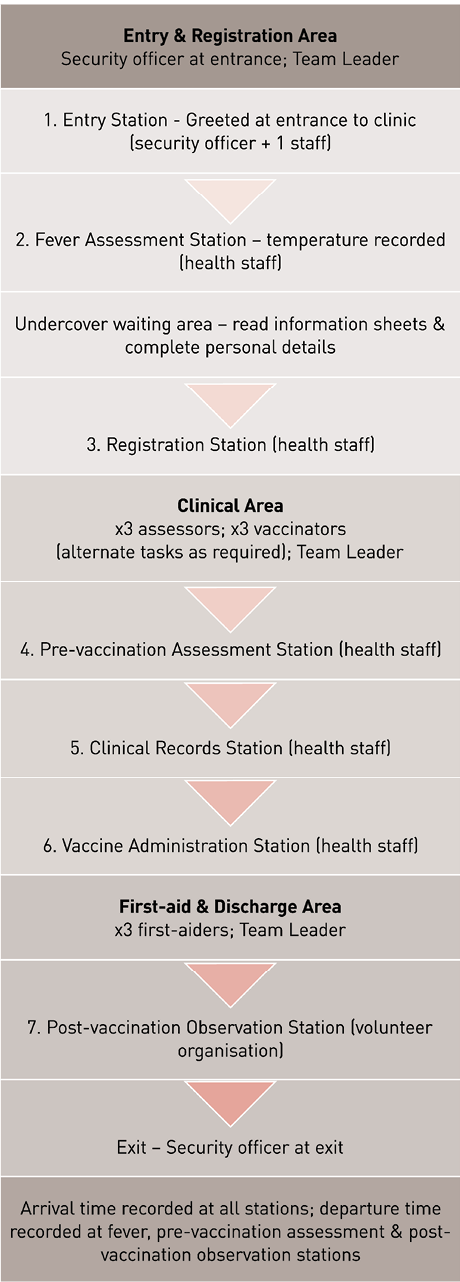
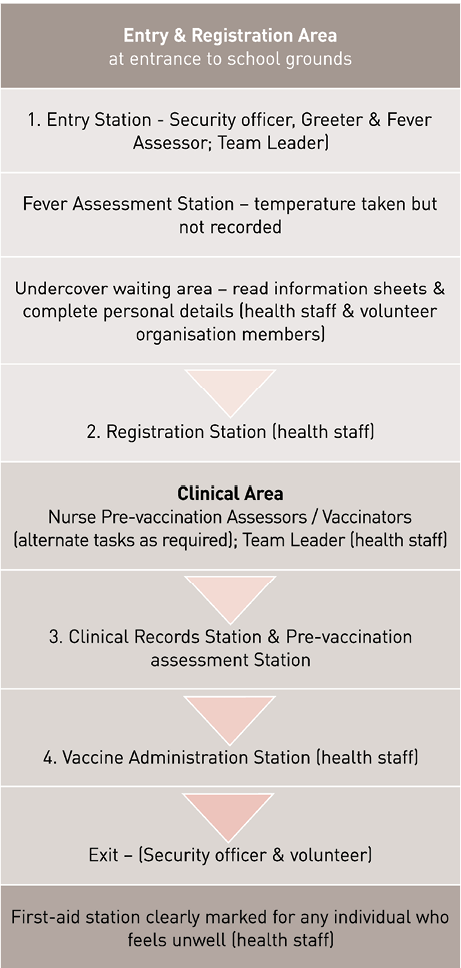
A community advertising campaign was initiated three weeks prior to the clinic through all local print and electronic media. It was clearly stated that besides being an opportunity to obtain free and current seasonal influenza vaccine the participants would also be involved in an exercise to test pandemic plans. The vaccination clinic was conducted on 11 March 2008 at the local high school between 14h00 and 20h00. The clinic framework utilised a reproducible pod (small team unit) structure to enable the expansion of the response to meet increasing numbers of community presentations. The school front entrance was used as the clinic entry point and each individual was directed and timed through seven stations as per the State Plan: (1) greet, (2) fever assessment, (3) registration, (4) pre-vaccination assessment, (5) clinical administration station, (6) vaccine administration and (7) post-vaccination observation and exit.
The clinic was staffed by nurse immunisers and other personnel from local rural health services, and members of local volunteer organisations. (Figure 1) Registered nurses rotated between the roles of vaccinator and pre-vaccination assessor to alleviate the repetitive nature of tasks and to maximise proficiency. Vaccines were provided in pre-filled syringes and were transported from the State Vaccine Centre to local vaccine storage facilities through the state’s existing vaccine transportation system which provides for specifically trained personnel to receive, store and monitor vaccines. Vaccines were monitored from point of dispatch to vaccine administration, to ensure cold-chain acceptability.
Figure 1: Flow of clinic operations used in Exercise as per existing Plan.
Three key aspects of the current Plan – effectiveness, safety, and client participation – were evaluated by seven evaluators who rotated through clinic stations hourly, using a standardised reporting tool for recording observations. Evaluators reviewed each clinic function against the effectiveness and efficiency of each position as described in pre-prepared Job Action Sheets.
Client satisfaction data were obtained using a semi-structured self-administered survey which was completed during the post-vaccination observation period. Exercise situation reports and briefings from the AARs captured data from the staff and volunteers involved in the exercise. Detailed time and flow analysis data were collected from each of the seven clinic stations using calibrated clocks to standardise arrival and departure times.
Quantitative data were analysed with Microsoft Excel and SPSS version 12 (IBM, 2005) Analysis included calculation of flow rates through specific vaccination stations and the conducting of a cohort analysis to identify “flow bottlenecks”.
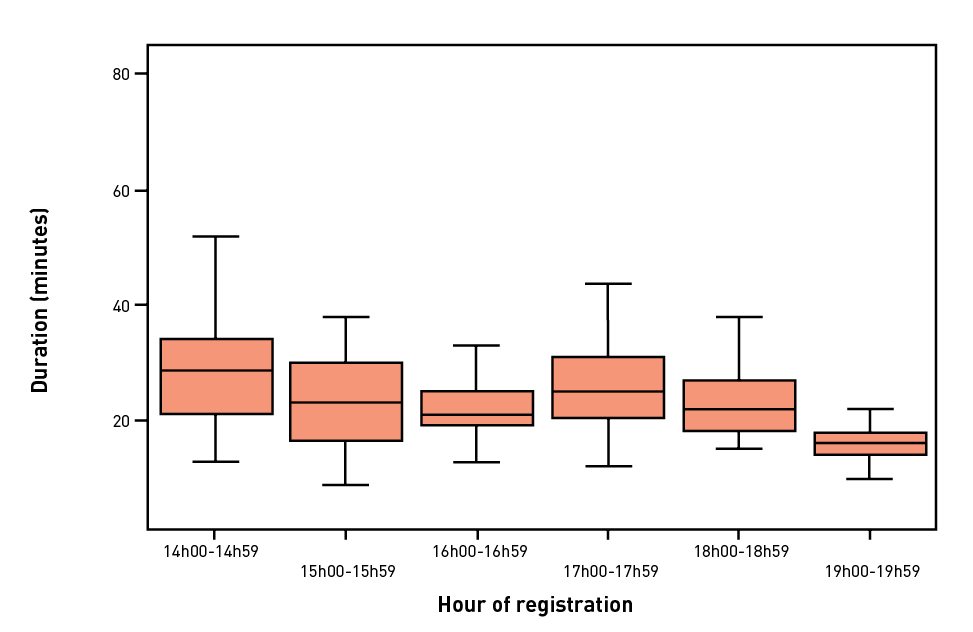
Four hundred and ninety eight clients were vaccinated at the clinic over the six hour period. The greatest number of presentations was seen in the first hour of the clinic (n=108) and an increase of adults was also noted between 17h00 and 19h00 coinciding with the end of shifts at local businesses and local news media coverage.
Standardised observations by umpires and AARs indicated that the chain of command and communication channels as described in the Plan were strictly adhered to by all staff during the clinic.
The current Team Leaders’ Job Action Sheets however did not adequately reflect the leadership role required to effectively manage the clinic operations and client flow. Umpires reported that client flow was managed in accordance with safe operational plans and that a school facility had the necessary infrastructure required for successful mass clinic deployment.
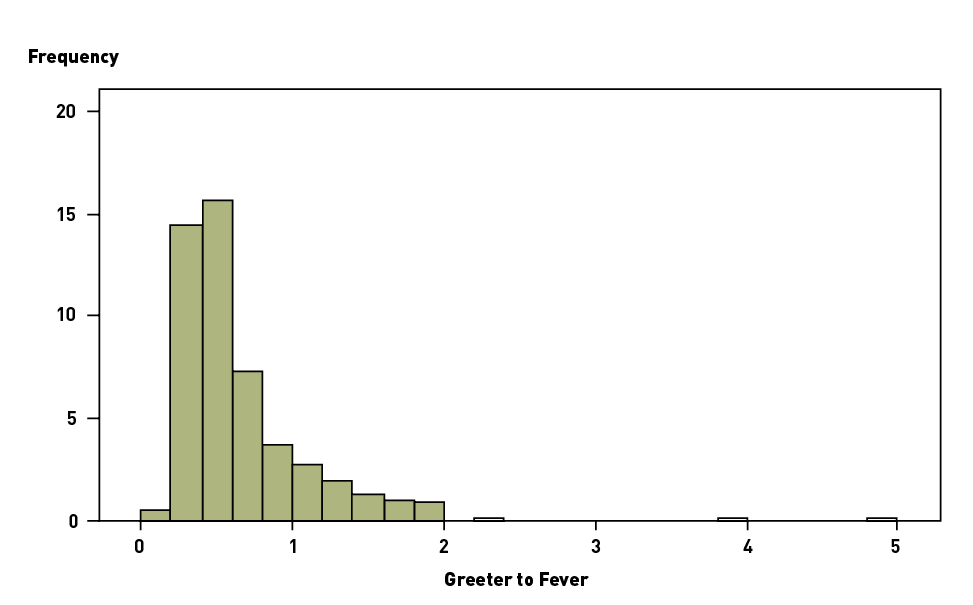
There was considerable variation in the movement through the various stages of the clinic which resulted in periodic bottle-necks during high throughput periods (Table 1). Although all transition times were positively skewed this was particularly pronounced for the time taken from greeter to fever assessor, which was the least actively shepherded transition (Figure 2).
Table 1: Time (in minutes) through clinic stations.
| Time (minutes) | Station 1-2 Greeter to Fever Assessment |
Station 2-3 Fever Assessment to Registration |
Station 3-4 Registration to Pre-Vaccination |
Station 4 Pre-Vaccination to Vaccination |
Station 5-6 Vaccination to Post- observation |
Station 1-6 Greeter to Post-observation |
|---|---|---|---|---|---|---|
| Median | 5 | 7 | 4 | 1 | 4 | 22 |
| IQR | 4 | 5 | 4 | 0 | 3 | 12 |
| Range | 49 | 26 | 15 | 7 | 16 | 78 |
| Maximum | 50 | 26 | 15 | 7 | 16 | 82 |
Figure 2. Time (in minutes) by each individual between Greeter and Fever Assessor.
Analysis of variance demonstrated statistically significant differences in median times between most stations during the clinic. The pre-vaccination assessment station was the most efficient. Of the 498 clients vaccinated at the clinic over the six hour period 81.1% (404) spent less than two minutes at the pre-vaccination station and 97.4% (485) spent less than three minutes. A third of clients (162) failed to leave after the appointed fifteen minutes post-vaccination observation period despite experiencing no vaccine adverse effects. Although there was an overall improvement in median time taken through the clinic for clients during the exercise there was still considerable variation (Figure 3).
Figure 3. Time (in minutes) from Greeter to arrival at Post-vaccination Observation.
Evaluators reported that clinic staff effectively activated the contingency plan for resource utilisation and surge staff when a need was identified, and staff members were effectively re-deployed to other tasks to meet changes in demand at specific stations.
No significant adverse event following vaccination and no safety incidents were reported during the exercise. One mild reaction following vaccination was self-limiting and required no treatment. Licensed security officers stationed at the entrance were observed to provide support to those clinic staff members who were isolated from the main clinic stations. Vaccinators were initially seated but after the first hour were requested by their Team Leader to stand in order to increase the throughput of their station. Some vaccinators subsequently reported leg and back strain after continual bending to sign vaccination record cards and service records.
Vaccine temperatures were observed by evaluators to be under continuous monitoring and were documented as satisfactory prior to and during clinic operations.
The self-administered satisfaction survey showed a high level of acceptance (98-99%) in all categories assessed: method of communication, clinic management, influenza and vaccine information, answers to questions posed by clients, treatment of clients by clinic staff, and waiting times. Ninety-nine percent of clients rated overall clinic management as excellent or good (482/489). Ninety-eight percent (472/484) of clients rated the information sheet provided on influenza as excellent or good, while 98% (479/488) of clients also rated information provided on influenza vaccination as excellent or good. Ninety-nine percent (482/485) of respondents regarded staff responses to their questions and concerns regarding the clinic, the vaccine or the disease, as excellent or good. Ninety-nine percent of participants (485/488) rated treatment by clinic staff as excellent or good. Most respondents indicated high satisfaction with waiting times, with 97% (472/488) considering this aspect as excellent or good.
The exercise proved valuable in evaluating the existing Mass Vaccination Clinic Plan and identifying opportunities to improve it. The exercise demonstrated that although the existing Plan could be operationalised safely there was considerable scope for improving efficiency. Streamlining the existing structure, functions, procedures and communications to enhance client flow, and enhancing the involvement of other agencies and volunteers, were identified as essential for improved throughput at future mass clinics. The school proved an ideal venue for deploying a mass clinic. Reducing the number of stations as described in Figure 4, limiting the physical distance between stations, and employing more rigorous marshalling of individuals to prevent straying, would improve efficiency and throughput.
Figure 4: Flow of revised clinic operations.
The high level of client compliance and satisfaction with the clinic process and waiting times may not be reflected in a pandemic situation when community anxiety is heightened, therefore in pandemic situations, enhanced queuing management, improved clinic signage outside and within the clinic building, and movable physical barriers to match demand, would improve clinic management and assist clients to move swiftly through the stations.
Following the AAR, Job Action Sheets for team leaders were modified to highlight their leadership role, specifically regarding enhancing communications and managing emerging situations. The consent and registration process should be streamlined by dispensing with documentation by both clients (written consent) and vaccinators (signing vaccination records).
Volunteers could effectively replace health staff for all but clinical roles (pre-vaccination assessors and vaccinators) which would minimise the burden on health services during a pandemic. Having the ability to re-deploy staff within the clinic to meet surge at particular stations positively impacted on client flow during the Exercise.
The short time spent in the pre-vaccination assessment station by most vaccinees suggests that the information sheet effectively addressed community concerns about the disease and the vaccine. The importance of ensuring that the community is well informed about pandemic influenza and the risks and benefits (including safety concerns) of a tailored pandemic vaccine cannot be overstated.
To further improve through-put, vaccinators’ role should be limited to vaccinating. Dispensing with the vaccinator’s requirement to document (date/batch numbers) and to sign record cards, would also reduce the occupational risk of back and limb fatigue for vaccinators.
With only one mild reaction following vaccination, together with the overwhelming evidence of the low incidence of immediate adverse events following vaccination in Australia over the past decade, it is reasonable to replace the observation station with a first-aid point for anyone feeling unwell. (Australian Government Department of Health and Ageing, 2008) This would increase the clinic’s capacity by preventing bottle-necks post-vaccination, while simultaneously reducing the risk of contact with undiagnosed cases of pandemic influenza.
This field exercise demonstrated inefficiencies in the current Mass Vaccination Plan. Key issues included the number and location of stations, formal consent and vaccinator documentation requirements, the lengthy post-vaccination observation period and the need for surge capacity that can be rapidly deployed to maintain clinic flow. The Exercise provided us with the opportunity to streamline existing plans and procedures after a practical evaluation. The lessons from this field exercise, the first of its kind in Australia, have the potential to improve future application of the mass vaccination clinic model should a second wave of pH1N1 occur or in the event of a large-scale public health response requiring mass administration of medications. (Durrheim, D., Ferson, M., 2006; Ferguson, N., et al, 2006)
Commander John Gralton, Upper Hunter Command, NSW Police (Chief Umpire)
Dr Paul Armstrong, Director, Biopreparedness Unit, NSW Health Department
Sue Campbell-Lloyd, Manager, Immunisation Unit, NSW Health Department
Josh Edmonds, Project Support Officer, Biopreparedness Unit, NSW Health Department,
Maree Lamb, Biopreparedness Officer, North Coast Area Health Service
Gosta Liljeqvist, Special Projects Officer, Biopreparedness Unit, NSW Health Department ,
Chabela Torres, Biopreparedness Epidemiologist, Northern Sydney Public Health Unit.
Aaby K., Cook, D., Herrmann, J., Jordan, C., Wood, K. (2008), Simulating a mass vaccination clinic: Health Care Management Science,
http://www.isr.umd.edu/Labs/CIM/projects/clinic/hcms.pdf (accessed Dec 30, 2008).
Australian Government Department of Health and Ageing (2008), The Australian Immunisation Handbook, 9th Edition, Canberra.
Australian Government Department of Health and Ageing (2009), Australian Health Management Plan for Pandemic Influenza; Commonwealth of Australia, Canberra.
Bishop, J. (2009), Managing Pandemic (H1N1) 2009 Influenza: A national health response, The Australian Journal of Emergency Management, Vol. 24, No.3, pp.5-6.
Durrheim, D., Ferson, M. (2006), Preparing for the inevitable – an influenza pandemic. NSW Public Health Bulletin, Vol. 17, pp. 97-98.
Eastwood, K., Durrheim, D.N., Massey, P.D., Kewley, C. (2009), Australia’s pandemic protect strategy: the tension between prevention and patient management. Rural and Remote Health 2009; 9: 1288.
Eastwood, K., Durrheim, D., Jones, A., Butler, A. (2009) Acceptance of Pandemic (H1N1) 2009 Influenza Vaccination by the Australian Public, Medical Journal of Australia, eMJA Rapid Online Publication 4 November 2009.
Ferguson, N., Cummings, D., Fraser, C., Cajka, J., Cooley, P., Burke, D. (2006), Strategies for mitigating an influenza pandemic. Nature, Vol. 442, pp. 448–452.
IBM (2005), Statistical Package for the Social Sciences for Window version 12. Illinois: Chicago.
New South Wales Health (2005), NSW Health Interim Influenza Pandemic Action Plan; NSW Government Printing, Sydney.
Philadelphia Department of Public Health Division of Disease Control, Bio-terrorism and Public Health Emergency Preparedness Consultants (2005), Roundtable Discussion After-Action Review of PDPH Dispensing Site Exercise October 14, 2005 Updated / Final-Report November 26, 2005, Emergency Management Innovations.
World Health Organization (2005), 2005 Global influenza preparedness plan, World Health Organization, Geneva.
World Health Organization (2008), Weekly Epidemiological Record southern hemisphere strain 2008.
Dr Christine Carr, PhD, M MedSc, PostgradDip MedSc, MRCN
At the time of the exercise Chris was Immunisation Coordinator with Population Health, Hunter New England Area Health Service, New South Wales, Australia. Chris, who has two decades of experience in immunisation management and education and has served on numerous State immunisation committees, led the field exercise coordinating group. She may be contacted at
chris.carr@hunterlink.net.au.
Prof David Durrheim, MBChB, MPH&TM, DTM&H, DCH, DrPH, FACTM, FAFPHM
Director of Health Protection, Public Health Physician and local Public Controller for disasters, Hunter New England Area Health Service, New South Wales, Australia. He is a member of the Strategic Advisory Group of Experts (SAGE) on Immunization to the World Health Organization and has extensive global experience in communicable disease control and immunisation.
Keith Eastwood, MAppEpid, BAppSci
Biopreparedness epidemiologist, Population Health, Hunter New England Area Health Service, New South Wales, Australia. Keith is currently undertaking doctoral studies in Public Health.
Peter Massey
With a nursing background, Peter is Program Manager in Communicable Diseases, Population Health, Hunter New England Area Health Service, New South Wales, Australia. Peter has extensive experience in immunisation, rural and Indigenous health service delivery and is currently undertaking doctoral studies in Public Health.
Dr Debbie Jaggers, PhD
Debbie is General Manager, Upper Hunter, Hunter New England Area Health Service, New South Wales, Australia. Debbie coordinated local capacity for the exercise.
Meredith Caelli, RN, BPSN, PostGradDip Biostatisitcs and Clinical Epidemiology
At the time of the exercise Meredith was Biopreparedness Officer, Disaster Response & Coordination Unit, Hunter New England Area Health Service, New South Wales, Australia. Meredith is currently undertaking doctoral studies in Community Medicine and Clinical Epidemiology
Sonya Nicholl, MPH, BSc (Hons) RGN
At the time of the exercise Sonya was Senior Policy Analyst, New South Wales Health Immunisation Unit, Australia. Sonya currently works as a Nursing Unit Manager for New South Wales Justice Health.
Linda Winn, MN, BN, Dip App Sci (Nursing)
At the time of the exercise Linda was Manager, Disaster Response & Coordination Unit, Hunter New England Area Health Service, New South Wales, Australia. Linda is currently the Deputy Director, New South Wales Health, Counter Disaster Unit.